Health insurance is a complex industry to navigate with myriads of hurdles in the form of processes tangled with regulations and age-old legacy systems. While automation has become the new normal in a world of digital business, health insurance has lagged behind. Even the technologically advanced payers are crippled with greater operational cost, poor customer experience, higher cycle time, and a tangled back office. It’s now time to run at the speed of new and evolving opportunities and fully embrace the power of intelligent automation.
With the above thought in mind, Coforge has built its healthcare intelligent automation capabilities leveraging our partnerships with Pega, UiPath, Automation Anywhere and Appian to automate processes in healthcare core areas of sales, quote to card, enrolment, consumer engagement, claims processing, referrals and authorisation, payment integrity, and case management – ultimately delivering a superior customer experience.
Intelligent Automation:
We approach automation holistically across business and IT processes through a host of solutions and services around the automation continuum including Robotic Process Automation (RPA), Robotic Desktop Automation (RDA), Intelligent Process Automation (IPA) and Artificial Intelligence (AI). Our deep knowledge of the healthcare industry and capabilities across the automation continuum enable us to align the right automation solution with client’s context using the following framework.
|
|
Data Type |
Processing |
Ability to Learn |
Context Awareness |
Approach |
| RDA(Assisted Automation) |
Structured |
Deterministic |
No |
No |
Human Triggers |
| RPA(Unassisted Automation) |
Structured and Semi Structured |
Deterministic |
No |
No |
Orchestrated Process Automation |
| IPA (Intelligent Automation) |
Structured and Semi Structured |
Probabilistic |
No |
Yes, but limited to environment |
Distributed Computing |
| AI (Cognitive Automation) |
Structured, Semi and Un-Structure |
Probabilistic |
Yes |
Yes, similar to Human Brain |
Machine Learning, Deep Learning, NLP |
Our services allow us to deliver a comprehensive mix of capabilities integrating class-leading partner products and our in-house capabilities. We bring best-in-class technologies, IPs, frameworks and solution accelerators to set the client on an incremental automation path towards delivering business outcomes and adding value. We also help existing and new clients develop an automation strategy focused on all key functional areas. Our proprietary ProcessGymTM framework allows us to take a very holistic and strategic approach towards delivering clear outcomes in any consulting and automation engagement.
Our expertise in developing, deploying, and operationalizing bots is the icing on the cake in this automation paradigm- be it a first level engagement in customer service or the more complex claims processing and adjudication, our bots can make it a breeze. We maintain an industry-leading certification standard that reinforces our partnerships with OEMs- having the highest percentage of certified resources across any Pega practice or being consistently ranked first in Appian’s A-Score program are testimonies to our partnership commitment.
Our in-house capabilities and partnerships let us bring in top-notch capabilities around BPM, case management, RPA, and CRM, allowing payers to deliver an unmatched customer experience with ease. Our healthcare industry knowledge aligns in concert with the technical expertise to tailor a solution package that works in harmony with the client’s existing systems.
Intelligent Automation for Healthcare Transformation:
Our automation capabilities have transformed enterprises spanning across industries, turning them into the smart organizations of the future. We firmly believe that intelligent automation technologies will continue to enable payers to deliver business agility, self-service enablement, and superior experiences. Automation has been a major enabler impacting Healthcare leading to cost take-outs and reinvestments in strategic areas, however, the automation approach is quite fragmented and silo-ed. We believe that there is a greater need to move away from these siloes to systematic automation of processes for handling scale without compromising on the quality and consistency of service.
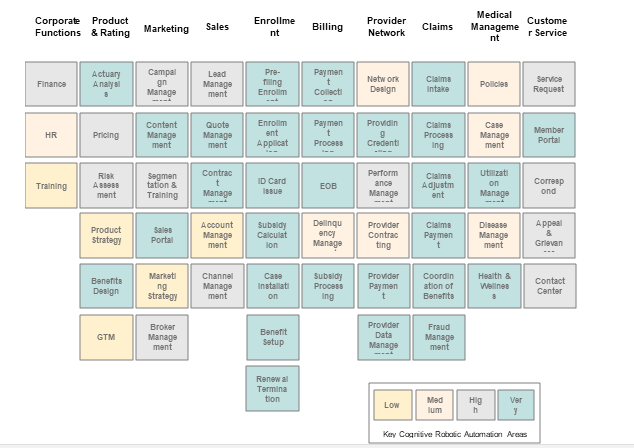
For healthcare payers, Automation can be leveraged in areas such as Product and Rating, Marketing and Sales, Member Enrolment, Billing, managing provider network, claims processing, and customer services. The following process heat map depicts a comprehensive list of areas where we can assist payers leveraging automation:
Intelligent Automation Use Cases for Healthcare Payers:
We address specific automation needs of customers while removing the dependency on a single proprietary platform/approach, which allows us to pick and choose from the best and tailor a bespoke solution and approach for your organization. Coforge has invested in a dedicated intelligent automation practice with its product experts and automation practitioners working in tandem with healthcare domain experts to drive enterprise automation roadmap and enable automation institutionalization. The practice also manages partnerships and alliances with OEM vendors and explores innovative automation technologies to serve our clients better.
Few of the payer use cases around which we have explored and built capabilities are-
- Provider Credentialing: Provider credentialing is a process of obtaining, verifying, and accessing the qualifications of a practitioner. Provider data, e.g. education, license, experience, certifications, affiliations, malpractice etc., needs to be accurately verified in order to enroll them to provide care or service to a health care organization. The manual credentialing process not only increases the chance for inaccurate validation but also affects the payer’s credibility. Inaccurate credentialing also impacts revenues and patient experience. Every payer organization needs a streamlined and automated credentialing process to avoid the above-mentioned challenges. Leveraging our RPA services, we can make sure that your provider data from different sources is verified and validated in an automated manner. The automation can also ensure that the latest provider data is used in this process, leading to minimized credentialing cycle time and enhanced provider onboarding experience.
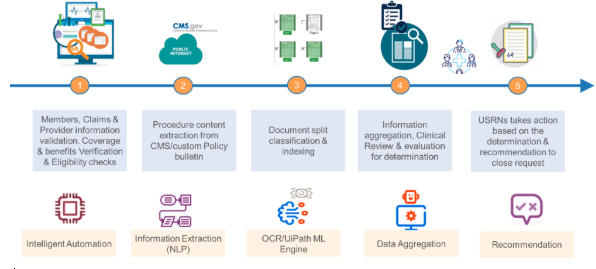
- Clinical Claim Review for Utilization Management: Our multiple solutions across the automation continuum can help a registered nurse (USRN) expedite the clinical claims review for Utilization management.
- Member Enrolment: Current enrolment process is time consuming and error prone as all the enrolment requests need to be validated & verified manually for all required information and data entry. The challenges faced in the process are
- Applicants missing precise information on the name, address, income, and other demographic and basic health information
- High turnaround time between submission and approval of an application
- Lack of a robust tracking mechanism for monitoring
We bring together multiple input channels such as email, shared folders, web portals managed by the bots for enrolment request data intake. Data can then be extracted from these sources and be validated as per the predefined business rules. Automation in member enrolment saves cost, increases process efficiency, can reduce administrative efforts by 75% and AHT (Average Handling Time) by 35-45%.
Related reads.


About Coforge.
We are a global digital services and solutions provider, who leverage emerging technologies and deep domain expertise to deliver real-world business impact for our clients. A focus on very select industries, a detailed understanding of the underlying processes of those industries, and partnerships with leading platforms provide us with a distinct perspective. We lead with our product engineering approach and leverage Cloud, Data, Integration, and Automation technologies to transform client businesses into intelligent, high-growth enterprises. Our proprietary platforms power critical business processes across our core verticals. We are located in 23 countries with 30 delivery centers across nine countries.


